Visit us in San Francisco
Academic standards. Pioneering research. Personalized care. Start your journey at the UCSF Center for Reproductive Health, located in Northern California's San Francisco Bay Area.
There are two different types of genetic tests that can be performed on embryos before they are implanted – preimplantation genetic testing for aneuploidy (PGT-A, previously known as PGS) and preimplantation testing for a monogenic disorder (PGT-M, previously known as PGD).
PGT-A is a screening test that evaluates the embryo’s chromosomes, the structures that hold all of our genetic material.
The correct number of chromosomes in an embryo is 46 – where half should come from the egg and the other half from the sperm. PGT-A screens for the presence of any missing or extra chromosome material, within the limits of test resolution. Chromosome abnormalities in an embryo may lead to failure of the embryo to implant, a miscarriage, or impact health of a future child. PGT-A does not change or correct the embryo’s chromosomes. However, if an embryo is screen normal through PGT-A, the risks previously described are lower than for an embryo that has not been screened.
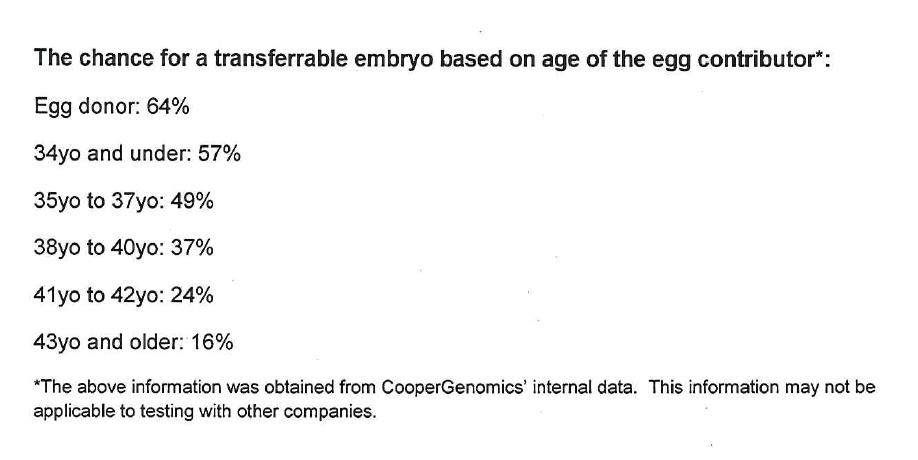
The primary factor that determines risk of abnormal chromosomes in an embryo or pregnancy is age of the egg contributor. The chart below shows estimated average chances for an embryo to have a normal PGT-A result, based on maternal age. Chromosome results vary between embryos and cycles, so these figures are not exact estimates for a cycle outcome. PGT-A can be performed in conjunction with a standard IVF cycle for any person or couple, but is typically considered in cases where the female partner is over 35 years of age. An additional benefit of PGT-A is that it improves our ability to choose the healthier embryos in a cohort, achieving an improved success rate with a single embryo transfer—when a normal embryo is identified through PGT-A—and reducing the risks of twin pregnancy. As PGT-A is a screening test, there is a possibility of misdiagnosis of the embryo's chromosomes.
Preimplantation genetic diagnosis or preimplantation genetic testing for monogenic (single gene) disorders (PGT-M) is a testing option that is available when there is a known genetic condition in a person or family. This test, when used in conjunction with IVF, can help to reduce the risk of passing on an inherited condition. It may be appropriate when both reproductive partners are identified to carry the same genetic condition (such as cystic fibrosis or sickle cell anemia), when there is a personal history of a genetic condition in one partner or a close relative, when a female patient is a carrier for a X-linked condition or when patient or partner carry a balanced chromosome rearrangement (PGT-SR). Families may also use PGD when a member of the family is in need of a bone marrow donor, as a way to have a child who can provide matching stem cells.

PGT-M is available for many inherited conditions for which the exact mutation is known. Because each case is unique, PGT-M involves case referral to a genetic laboratory, which must then usually build a custom test. This process typically takes about 3 months in total, before an IVF cycle can begin.
PGT-M can significantly reduce the chances of having a child with the condition. It is typically done for couples that do not have difficult conceiving. Many couples know they are at risk due to a family member with the disease, but some people or couples may be silent carriers. Preconception carrier screening can help to identify some people and couples at increased risk of having a child with a genetic condition, and PGT-M may become an option for them during the course of their care with us.
There are multiple types of preimplantation genetic testing (PGT). Your physician can help you determine what type of testing may be appropriate or recommended for you.
Academic standards. Pioneering research. Personalized care. Start your journey at the UCSF Center for Reproductive Health, located in Northern California's San Francisco Bay Area.