Visit us in San Francisco
Academic standards. Pioneering research. Personalized care. Start your journey at the UCSF Center for Reproductive Health, located in Northern California's San Francisco Bay Area.
We are currently booking new patient appointments. Please fill out our form to get started.
Recurrent pregnancy loss (RPL) is defined as the miscarriage of two or more clinical pregnancies.
The risk of a single miscarriage ranges from 15% to 50% or more per pregnancy, depending on a woman’s age, and is most often due to abnormal chromosome content in the pregnancy. In contrast, approximately 1-2% of couples suffer from RPL.
Known risk factors for RPL include:
RPL is an emotionally challenging experience. Frustratingly, up to 50% will have no cause identified after a thorough workup (“unexplained RPL”). The reproductive endocrinologists at UCSF are trained specialists in the area of recurrent pregnancy loss and are committed to providing an evidence-based approach to workup and treatment options for family building.
Our team of interdisciplinary experts at the Center for Reproductive Health is also committed to advancing the science for patients with recurrent pregnancy loss everywhere. To this end, we are launching the UCSF Multidisciplinary Recurrent Pregnancy Loss Center which will offer a comprehensive opportunity to be seen by reproductive endocrinologists, psychologists and genetic counselors for a thorough evaluation and management plan – and to partner with us in advancing knowledge about RPL by participating in research studies.
In approximately 4% of couples who experience RPL, one or both partners will have an abnormality of chromosome structure. In such cases, one possible therapy is in vitro fertilization (IVF) with preimplantation genetic testing of the embryos (PGT).
Abnormalities of the uterine cavity account for approximately 15-20% of cases of RPL. Abnormalities may include a uterine septum, uterine scar tissue, polyps or fibroids. Diagnostic tests such as saline sonograms and hysteroscopy can be used to evaluate the uterine cavity. Many abnormalities within the uterus can be corrected with minimally invasive surgery called hysteroscopy.
In approximately 15% of couples with RPL, the cause may be related to antibodies that interfere with the pregnancy’s development. Blood tests are performed to make a diagnosis of anti-phospholipid antibody syndrome (APS). APS has been shown to respond to treatment with blood thinners.
Women with uncontrolled diabetes mellitus and uncorrected thyroid-gland dysfunction are at an elevated risk of miscarriage. Correction of hormonal imbalances is recommended in these cases.
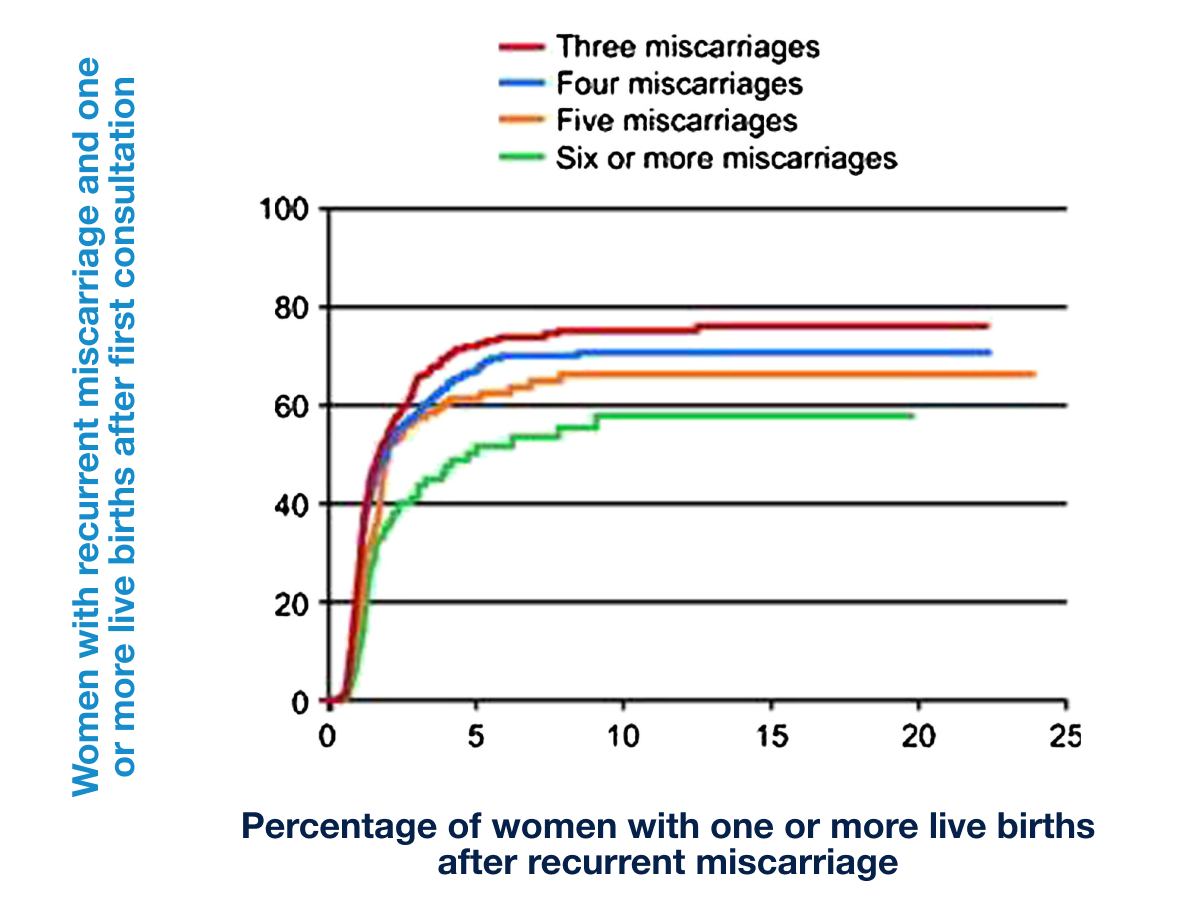
The prognosis for a future live birth remains optimistic for many couples with recurrent pregnancy loss. Depending on female age and number of prior losses, chances for a live birth in subsequent pregnancies may range from 40%-80%.
Academic standards. Pioneering research. Personalized care. Start your journey at the UCSF Center for Reproductive Health, located in Northern California's San Francisco Bay Area.
Academic standards. Pioneering research. Personalized care. Start your journey at the UCSF Center for Reproductive Health, located in Northern California's San Francisco Bay Area.






